Childhood obesity remains a critical global public health issue, particularly due to its long-term health risks and rising prevalence. This study highlights the significance of Motor Quotient (MQ) physical fitness training as an effective intervention for improving health-related fitness indicators in obese children aged 7–8 years. By demonstrating significant improvements in key fitness metrics such as agility, strength, and flexibility after a structured 13-week MQ program, this research underscores its practical implications for combating childhood obesity within school environments. Theoretically, it contributes new insights into the relationship between targeted fitness programs and obesity-related health variables, offering a valuable framework for early intervention strategies in similar populations. These findings emphasize the need for further research with larger samples to explore the long-term impact and scalability of MQ training in diverse educational settings.
Designing MQ training programs to improve physical fitness in obese children
Obesity among children has emerged as a serious public health threat, increasing morbidity risk while simultaneously diminishing quality of life. Studies demonstrate the devastating consequences of sedentary lifestyles on this population’s physical development, with numerous reports documenting its negative influence. Studies confirming its detrimental impact both physically and psychosocially are numerous. Zongping Wang’s Motor Quotient (MQ) training program serves as the cornerstone for improving physical fitness of obese children. This program stresses the significance of recognizing and developing students’ motor quotient to unlock their athletic potential, advocating the necessity of consistent physical activity as part of an overall sports culture that honors life-long participation (20). The MQ Training program represents an innovative solution to increase multidimensional physical fitness while decreasing child obesity. Optimizing the design and delivery of such programs merits further discussion, particularly as regards meeting the unique needs of obese pediatric cohorts. A key design principle should be targeting specific aspects of fitness that have been most compromised due to obesity. Obese children tend to show reduced strength, motor skills, agility, flexibility and cardiovascular endurance compared with their leaner peers (33, 34). Combining continuous aerobic activity to increase peak VO2, along with resistance training, motor skills exercises, and stretching as part of an integrated fitness approach offers a strategic way of combatting obesity-related fitness deficits (35). Beyond fitness outcomes, MQ programming must address the negative psychosocial correlates of pediatric obesity to maximize adherence and health benefits. Obese children are disproportionately prone to low self-efficacy, negative body image, and peer victimization, all of which militate against participation in physical activity (36). Sensitively structured sessions that focus on enjoyment, inclusion, and cooperation can overcome these barriers, as can family-based initiatives to cultivate support (37). Key design considerations of MQ obesity interventions for MQ cohorts should center around optimizing training frequency, intensity and duration – though no consensus exists as of yet regarding optimal sessions for obese cohorts, it appears 3–5 weekly 30- to 60-minute training sessions may provide the greatest return (38). Moderate-to-vigorous intensity, eliciting 60–90% of maximal heart rate, prevents overexertion while stimulating cardiorespiratory and metabolic adaptations (39). Such programming parameters help to strike a balance between efficacy and feasibility. In this context, the Motor Quotient (MQ) training program, as highlighted by Zongping Wang, emphasizes the recognition of the motor quotient to enhance the athletic potential of Chinese children, emphasize the importance of regular physical activity, and promote a culture of lifelong sports participation. The design of the training program within the MQ paradigm was carefully tailored to address both the physical fitness and MQ assessments. The physical fitness assessment consisted of a series of seven observational measures, namely body mass index (BMI), a 2 × 30 m shuttle run, a one-minute jump rope, a plank hold, a seated forward bend, an in-place medicine ball throw, and a 20 m backward run. These tests were carefully selected to provide a comprehensive assessment of the children’s physical abilities, such as strength, speed, endurance, coordination, and flexibility, thus providing a nuanced understanding of their fitness profiles (40). Recent research by Xu et al. has described a non-linear relationship between weight status and physical fitness, showing that both underweight and obese children and adolescents have lower levels of physical fitness compared to their normal weight counterparts, underscoring the complexity of the relationship between body composition and physical performance (41). The MQ training program is not monolithic, but rather consists of a variety of modalities, including both dynamic and isometric exercises, carefully curated to enhance coordination and agility. This multifaceted approach has borne fruit, as evidenced by significant improvements in lower extremity, upper extremity, and core strength. Accompanying these physical improvements were observable gains in coordination and agility, which may collectively contribute to increased physical fitness and enriched quality of life for the obese pediatric cohort. These findings lend credence to the proposition that integrated training methodologies are instrumental in mitigating the challenges posed by childhood obesity.
Overall, MQ training program represents an innovative paradigm shift in its approach to childhood obesity by going beyond traditional exercise programs to foster holistic development of physical and motor skills. Empirical evidence collected so far supports expansion and continuation of such programs to bring significant and long-lasting improvements in children with obesity’s health trajectories.
The effect of MQ training programs on BMI in obese children
According to the results of this study, exercise program has shown some effect in improving children’s BMI, as well as potentially having a positive impact on children’s cognitive and learning abilities at that age.
This study suggests that training methods based on basic motor skills such as running backwards, jumping rope and throwing a solid ball may be more advantageous in improving children’s physical and mental ability to perform specific movements, but there is a lack of direct evidence that these methods are more effective than other training programs. This is because interventions in relevant studies typically include multiple training modalities, and the effectiveness of each training method has not been compared individually.
These activities focus on fundamental motor skills crucial for children’s physical development, making them more accessible and impactful in this age group (Table 5). In contrast, team-based, rule-bound programs like the Lucky Spin, which require a deeper understanding and processing of information and rely on collaborative efforts, may not be as effective within the constraints of limited classroom practice. Research indicates that insufficient physical activity, especially in conjunction with obesity, can lead to poor health-related fitness and reduced confidence in participating in sports and physical activities (42, 43). However, enhancing motor skills through tailored physical activities can boost a child’s motivation for physical engagement, often accompanied by improved self-esteem and enjoyment (44).
The impact of various exercise interventions on Body Mass Index (BMI) in obese children highlights the efficacy of activities that focus on enhancing fundamental motor skills appropriate for their age group. The study showed that individual exercises, such as the 20 m backward run and the one-minute rope skipping, significantly outperformed multiple program combinations. These exercises, which require singular execution, place high demands on specific physical attributes that are crucial at this developmental stage. The importance of various types of exercises, including weight lifting and aerobic exercise, in positively impacting BMI is well established (45). This is further supported by a pilot randomized controlled trial, which found that either caloric restriction alone or combined with rope-skipping exercise significantly reduced weight, BMI, PBF, and BFM in young adults over eight weeks (46). This underscores the role of targeted exercise in improving cardiometabolic health. In the context of this study, the one-minute rope skipping, which demands power and agility, effectively exercised these attributes, leading to significant effects in test outcomes. This suggests that the observed reduction in BMI among obese children is not solely due to a particular exercise, but rather the overall enhancement of physical qualities such as muscular strength and coordination. By engaging in rope skipping, children were able to improve these skills comprehensively, which in turn facilitated greater proficiency in activities requiring strength and coordination. This not only contributed to weight management but also aided in lowering BMI. In summary, the key to reducing BMI in obese children lies in advancing their physical capacities through targeted training that focuses on essential motor skills and attributes, rather than merely participating in specific types of exercises.
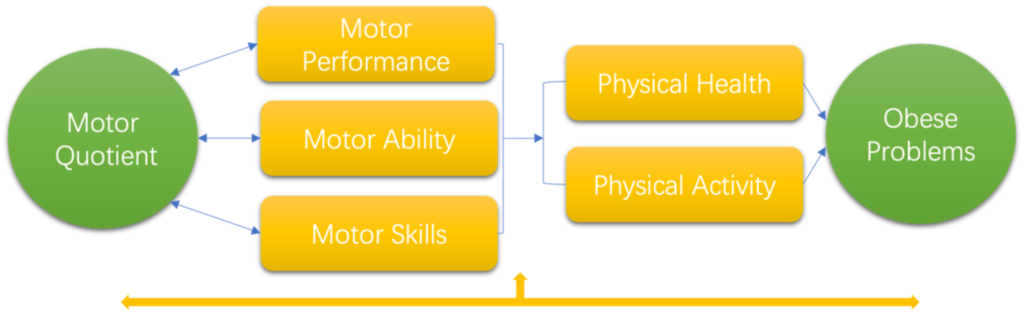
Regarding BMI calculations, they were derived directly from height and weight measurements in the study. The minimal changes in height observed among most children during the intervention period suggest that BMI changes were primarily due to weight fluctuations. Research indicates that obese children often have poorer physical coordination due to their excess weight, which can impede their ability to engage effectively in physical activities (47). Moreover, while physical activity is crucial for developing basic motor skills in younger children, the association between BMI and these skills, or physical activity levels, may not be as pronounced in preschoolers (48). Regression and correlation analyses in the study showed that exercises focusing on a single physical quality had a more significant impact on BMI than those involving multiple qualities. This is likely because exercises demanding multiple skills require synchronized mastery of diverse physical capacities, which can vary in development among obese children. In our study, we also found that behavioral tasks were significantly correlated with BMI, which is consistent with previous findings in the category of motor performance. Obese children’s motor skills and performance can be compromised to some extent due to body shape limitations (34), which can adversely affect sports participation and increased physical activity in obese children.(Fig. 1).
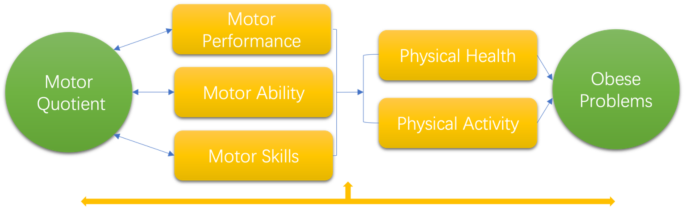
Relation between motor quotient and obese problems
The effect of school physical education on childhood obesity
In recent years, research has shown that methods such as High Intensity Interval Training (HIIT) and Tabata training in school physical education programs have significant potential to improve childhood obesity. These training methods are not only effective in reducing body fat in obese children, but also in improving their overall health. Tabata training, a high-intensity interval training method that alternates short bursts of high-intensity exercise with brief periods of rest, has been shown to have a significant effect on improving body composition and health-related fitness in obese children. For example, a study by Domaradzki et al. (2020) (49) demonstrated that Tabata training significantly reduced body weight, body fat percentage, and waist-to-hip ratio in overweight adolescents, while improving their aerobic capacity. A study by Popowczak et al. (2022) (50) also found that 10 weeks of Tabata training significantly improved body fat percentage and cardiovascular efficiency in 16-year-old middle school students. These findings suggest that Tabata training is not only effective in reducing body fat in obese children, but also in improving their overall health. In addition to Tabata training, other forms of high-intensity interval training (HIIT) have also shown positive effects on obese children. A systematic review and meta-analysis by Costigan et al. (2015) (51) showed that HIIT had significant effects in improving cardiorespiratory endurance and body fat in adolescents. In particular, for overweight and obese children, HIIT significantly reduced body fat percentage while improving cardiorespiratory fitness. These findings further confirm the effectiveness of HIIT in improving health-related fitness in obese children. Despite the significant potential of HIIT and Tabata training to improve the health of obese children, there are still some challenges to its implementation in school physical education program. For example, Liu et al.‘s (2024) (52) systematic review and meta-analysis noted that HIIT interventions in school physical education curricula have deficiencies in process evaluation, with many studies under-reporting details of the intervention process. This may have affected the accurate assessment and replication of intervention effects. Therefore, future studies need to focus more on process evaluation, including the implementation of the intervention, mechanisms of influence and contextual factors, in order to improve the feasibility and effectiveness of the intervention. In addition, research should also focus on the potential impact of these training methods on children’s mental health, such as self-esteem, anxiety and depression. By considering both physical and mental health together, the potential of these training methods in improving childhood obesity can be more fully assessed. Research should also focus on the individualization of training methods and gender differences to ensure that training programs are better adapted to the needs of different children.
In this study, we identified three major limitations. First, sample size limitations had an impact on our findings. As this study was part of an exercise participation intervention study under the MQ perspective, obese subjects participated in the MQ physical education program with normal weight subjects. This setting was designed to assess the variability of the intervention effects of the MQ physical education program on different weight groups. Although we have found the effectiveness of the intervention on BMI, Behavioral task, etc. in obese children in our study, to assess the effectiveness of the intervention more accurately for a group of obese children in future studies, we plan to implement a more customized MQ obesity intervention training program or curriculum design in a larger sample group. Second, the limitations of the assessment instruments are also a noteworthy issue. In monitoring weight changes in obese children, we only used BMI as a measurement tool due to operational limitations. Thirdly, as the interventions in this study included multiple means of exercise and the effectiveness of each means of exercise was not compared individually, it was not possible to directly demonstrate that a single means of exercise (e.g., running backwards, skipping rope, solid ball, etc.) was more effective than a combination of exercises. In future studies, further stratified analyses should be done to compare the effects of different combinations of exercise programs on the BMI of obese children to assess the independent effect of single exercise.
In addition, we only used target heart rate as an indicator of training intensity during the intervention. To obtain more comprehensive assessment results, future studies should consider incorporating relevant physiological indicators such as maximal oxygen uptake and motor function for more comprehensive monitoring and assessment of intervention effects.