Krasopoulos, G., Dusmet, M., Ladas, G. & Goldstraw, P. Nuss procedure improves the quality of life in young male adults with pectus excavatum deformity. Eur. J. Cardiothorac. Surg. 29 (1), 1–5 (2006).
Google Scholar
Lawson, M. L. et al. A pilot study of the impact of surgical repair on disease-specific quality of life among patients with pectus excavatum. J. Pediatr. Surg. 38 (6), 916–918 (2003).
Google Scholar
Roberts, J., Hayashi, A., Anderson, J. O., Martin, J. M. & Maxwell, L. L. Quality of life of patients who have undergone the Nuss procedure for pectus excavatum: preliminary findings. J. Pediatr. Surg. 38 (5), 779–783 (2003).
Google Scholar
Tardy, M. M. et al. Exercise cardiac output limitation in pectus excavatum. J. Am. Coll. Cardiol. 66 (8), 976–977 (2015).
Google Scholar
Rodriguez-Granillo, G. A. et al. Impact of pectus excavatum on cardiac morphology and function according to the site of maximum compression: Effect of physical exertion and respiratory cycle. Eur. Heart J. Cardiovasc. Imaging. 21 (1), 77–84 (2020).
Google Scholar
Abu-Tair, T. et al. Impact of pectus excavatum on cardiopulmonary function. Ann. Thorac. Surg. 105 (2), 455–460 (2018).
Google Scholar
Obermeyer, R. J., Cohen, N. S. & Jaroszewski, D. E. The physiologic impact of pectus excavatum repair. Semin Pediatr. Surg. 27 (3), 127–132 (2018).
Google Scholar
Swanson, J. W. et al. Correlating Haller index and cardiopulmonary disease in pectus excavatum. Am. J. Surg. 203 (5), 660–664 (2012).
Google Scholar
Maagaard, M. & Heiberg, J. Improved cardiac function and exercise capacity following correction of pectus excavatum: A review of current literature. Ann. Cardiothorac. Surg. 5 (5), 485–492 (2016).
Google Scholar
Coln, E., Carrasco, J. & Coln, D. Demonstrating relief of cardiac compression with the Nuss minimally invasive repair for pectus excavatum. J. Pediatr. Surg. 41 (4), 683–686 (2006). discussion – 6.
Google Scholar
Kelly, R. E. Jr. et al. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study. Pediatrics 122 (6), 1218–1222 (2008).
Google Scholar
Lomholt, J. J., Jacobsen, E. B., Thastum, M. & Pilegaard, H. A prospective study on quality of life in youths after pectus excavatum correction. Ann. Cardiothorac. Surg. 5 (5), 456–465 (2016).
Google Scholar
Jeong, J. Y., Park, H. J., Lee, J., Park, J. K. & Jo, K. H. Cardiac morphologic changes after the Nuss operation for correction of pectus excavatum. Ann. Thorac. Surg. 97 (2), 474–478 (2014).
Google Scholar
Lawson, M. L. et al. Impact of pectus excavatum on pulmonary function before and after repair with the Nuss procedure. J. Pediatr. Surg. 40 (1), 174–180 (2005).
Google Scholar
Maagaard, M. et al. Normalized cardiopulmonary exercise function in patients with pectus excavatum three years after operation. Ann. Thorac. Surg. 96 (1), 272–278 (2013).
Google Scholar
Malek, M. H. et al. Cardiovascular function following surgical repair of pectus excavatum: A metaanalysis. Chest 130 (2), 506–516 (2006).
Google Scholar
Redlinger, R. E. Jr. et al. Regional chest wall motion dysfunction in patients with pectus excavatum demonstrated via optoelectronic plethysmography. J. Pediatr. Surg. 46 (6), 1172–1176 (2011).
Google Scholar
Caspersen, C. J., Powell, K. E. & Christenson, G. M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public. Health Rep. 100 (2), 126–131 (1985).
Google Scholar
Das, B. B., Recto, M. R. & Yeh, T. Improvement of cardiopulmonary function after minimally invasive surgical repair of pectus excavatum (Nuss procedure) in children. Ann. Pediatr. Cardiol. 12 (2), 77–82 (2019).
Google Scholar
Borowitz, D. et al. Pulmonary function and exercise response in patients with pectus excavatum after Nuss repair. J. Pediatr. Surg. 38 (4), 544–547 (2003).
Google Scholar
Cebeci, H. et al. The effect of pectus excavatum deformity on lung volume: Fact or myth? Surg. Radiol. Anat. 42 (11), 1287–1292 (2020).
Google Scholar
Raghuveer, G. et al. Cardiorespiratory fitness in youth: an important marker of health: A scientific statement from the American heart association. Circulation 142 (7), e101–e18 (2020).
Google Scholar
Shephard, R. J. et al. The maximum oxygen intake. An international reference standard of cardiorespiratory fitness. Bull. World Health Organ. 38 (5), 757–764 (1968).
Google Scholar
Ross, R. et al. Importance of assessing cardiorespiratory fitness in clinical practice: A case for fitness as a clinical vital sign: A scientific statement from the American heart association. Circulation 134 (24), e653–e99 (2016).
Google Scholar
Coughlin, A. C. et al. When to nuss?? Patient age as a risk factor for complications of minimally invasive repair of pectus excavatum: A systematic review and meta-analysis. Pediatr. Surg. Int. 38 (3), 365–375 (2022).
Google Scholar
Media, A. S. et al. Complication rates rise with age and Haller index in minimally invasive correction of pectus excavatum: A high-volume, single-center retrospective cohort study. J. Thorac. Cardiovasc. Surg. (2024).
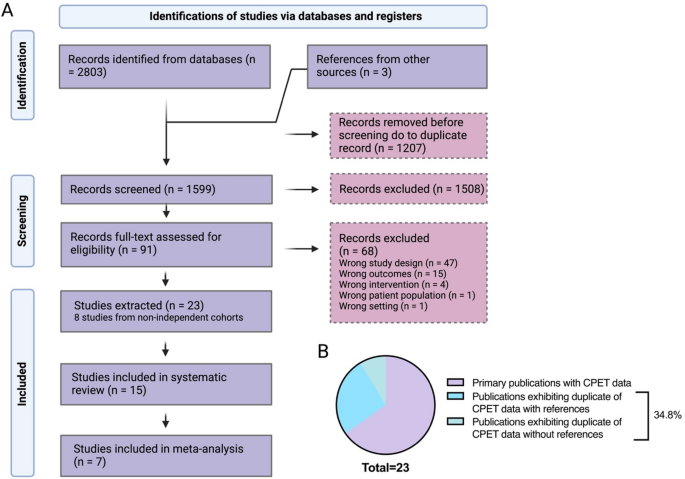
Moher, D. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4 (1), 1 (2015).
Google Scholar
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj 372, n71 (2021).
Google Scholar
Christopher, B., Cooper, M. A., Saleh, R., Elashoff, R. & Finn, J. P. Eric W. Fronkalsrud. Anatomical and physiological improvements following surgical correction of pectus excavatum: A prospective study. D42 Interventional Pulmonology and Thoracic Surgery 2010. p. A5841–A .
Poole, D. C. & Jones, A. M. Measurement of the maximum oxygen uptake V̇o(2max): V̇o(2peak) is no longer acceptable. J. Appl. Physiol. (1985). 122 (4), 997–1002 (2017).
Google Scholar
Thornton, A. & Lee, P. Publication bias in meta-analysis: Its causes and consequences. J. Clin. Epidemiol. 53 (2), 207–216 (2000).
Google Scholar
Haller, J. A. Jr. & Loughlin, G. M. Cardiorespiratory function is significantly improved following corrective surgery for severe pectus excavatum. Proposed treatment guidelines. J. Cardiovasc. Surg. (Torino). 41 (1), 125–130 (2000).
Google Scholar
Wurtz, A. et al. Simplified open repair for anterior chest wall deformities. Analysis of results in 205 patients. Orthop. Traumatol. Surg. Res. 98 (3), 319–326 (2012).
Google Scholar
Bawazir, O. A., Montgomery, M., Harder, J. & Sigalet, D. L. Midterm evaluation of cardiopulmonary effects of closed repair for pectus excavatum. J. Pediatr. Surg. 40 (5), 863–867 (2005).
Google Scholar
Sigalet, D. L., Montgomery, M. & Harder, J. Cardiopulmonary effects of closed repair of pectus excavatum. J. Pediatr. Surg. 38 (3), 380–385 (2003). discussion – 5.
Google Scholar
Sigalet, D. L. et al. Long term cardiopulmonary effects of closed repair of pectus excavatum. Pediatr. Surg. Int. 23 (5), 493–497 (2007).
Google Scholar
Al-Assiri, A. et al. Operative innovation to the Nuss procedure for pectus excavatum: Operative and functional effects. J. Pediatr. Surg. 44 (5), 888–892 (2009).
Google Scholar
Tang, M. et al. Improved cardiopulmonary exercise function after modified Nuss operation for pectus excavatum. Eur. J. Cardiothorac. Surg. 41 (5), 1063–1067 (2012).
Google Scholar
Ravanbakhsh, S. et al. Sex differences in objective measures of adult patients presenting for pectus excavatum repair. Ann. Thorac. Surg. 114 (4), 1159–1167 (2022).
Google Scholar
Wynn, S. R. et al. Exercise cardiorespiratory function in adolescents with pectus excavatum. Observations before and after operation. J. Thorac. Cardiovasc. Surg. 99 (1), 41–47 (1990).
Google Scholar
Quigley, P. M., Haller, J. A. Jr., Jelus, K. L., Loughlin, G. M. & Marcus, C. L. Cardiorespiratory function before and after corrective surgery in pectus excavatum. J. Pediatr. 128 (5 Pt 1), 638–643 (1996).
Google Scholar
Jaroszewski, D. E. et al. Cardiopulmonary outcomes after the Nuss procedure in pectus excavatum. J. Am. Heart Assoc. 11 (7), e022149 (2022).
Google Scholar
Neviere, R., Benhamed, L., Duva Pentiah, A. & Wurtz, A. Pectus excavatum repair improves respiratory pump efficacy and cardiovascular function at exercise. J. Thorac. Cardiovasc. Surg. 145 (2), 605–606 (2013).
Google Scholar
O’Keefe, J. et al. Longer term effects of closed repair of pectus excavatum on cardiopulmonary status. J. Pediatr. Surg. 48 (5), 1049–1054 (2013).
Google Scholar
Morshuis, W. J. et al. Exercise cardiorespiratory function before and one year after operation for pectus excavatum. J. Thorac. Cardiovasc. Surg. 107 (6), 1403–1409 (1994).
Google Scholar
Del Frari, B. et al. The questionable benefit of pectus excavatum repair on cardiopulmonary function: a prospective study. Eur. J. Cardiothorac. Surg. 61 (1), 75–82 (2022).
Cahill, J. L., Lees, G. M. & Robertson, H. T. A summary of preoperative and postoperative cardiorespiratory performance in patients undergoing pectus excavatum and carinatum repair. J. Pediatr. Surg. 19 (4), 430–433 (1984).
Google Scholar
Kelly, R. E. Jr. et al. Multicenter study of pectus excavatum, final report: Complications, static/exercise pulmonary function, and anatomic outcomes. J. Am. Coll. Surg. 217 (6), 1080–1089 (2013).
Google Scholar
Udholm, S., Maagaard, M., Pilegaard, H. & Hjortdal, V. Cardiac function in adults following minimally invasive repair of pectus excavatum. Interact. Cardiovasc. Thorac. Surg. 22 (5), 525–529 (2016).
Google Scholar
Tanaka, H., Monahan, K. D. & Seals, D. R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 37 (1), 153–156 (2001).
Google Scholar
Cicone, Z. S., Holmes, C. J., Fedewa, M. V., MacDonald, H. V. & Esco, M. R. Age-Based prediction of maximal heart rate in children and adolescents: A systematic review and Meta-Analysis. Res. Q. Exerc. Sport. 90 (3), 417–428 (2019).
Google Scholar
Neviere, R. et al. Cardiopulmonary response following surgical repair of pectus excavatum in adult patients. Eur. J. Cardiothorac. Surg. 40 (2), e77–82 (2011).
Google Scholar
Poston, P. M. et al. The correction index: setting the standard for recommending operative repair of pectus excavatum. Ann. Thorac. Surg. 97 (4), 1176–1179 (2014). discussion 9–80.
Google Scholar
Castellani, C., Windhaber, J., Schober, P. H. & Hoellwarth, M. E. Exercise performance testing in patients with pectus excavatum before and after Nuss procedure. Pediatr. Surg. Int. 26 (7), 659–663 (2010).
Google Scholar
Julious, S. A. Sample sizes for clinical trials with normal data. Stat. Med. 23 (12), 1921–1986 (2004).
Google Scholar
Arena, R., Myers, J. & Kaminsky, L. A. Revisiting age-predicted maximal heart rate: Can it be used as a valid measure of effort? Am. Heart J. 173, 49–56 (2016).
Google Scholar
Neviere, R. & Wurtz, A. Longer term effects of closed repair of pectus excavatum on cardiopulmonary status. J. Pediatr. Surg. 48 (9), 1988–1989 (2013).
Google Scholar
Gürkan, U. et al. Echocardiographic assessment of right ventricular function before and after surgery in patients with pectus excavatum and right ventricular compression. Thorac. Cardiovasc. Surg. 62 (3), 231–235 (2014).
Google Scholar
Krueger, T. et al. Cardiac function assessed by transesophageal echocardiography during pectus excavatum repair. Ann. Thorac. Surg. 89 (1), 240–243 (2010).
Google Scholar
Dunning, J. et al. The pectus care guidelines: Best practice consensus guidelines from the joint specialist societies SCTS/MF/CWIG/BOA/BAPS for the treatment of patients with pectus abnormalities. Eur. J. Cardiothorac. Surg. ;66(1). (2024).
Lundby, C., Montero, D. & Joyner, M. Biology of VO(2) max: Looking under the physiology lamp. Acta Physiol. (Oxf). 220 (2), 218–228 (2017).
Google Scholar
Montero, D., Diaz-Cañestro, C. & Lundby, C. Endurance training and V˙O2max: Role of maximal cardiac output and oxygen extraction. Med. Sci. Sports Exerc. 47 (10), 2024–2033 (2015).
Google Scholar
Lundby, C. & Robach, P. Performance enhancement: What are the physiological limits? Physiol. (Bethesda). 30 (4), 282–292 (2015).
Google Scholar
Bassett, D. R. Jr. & Howley, E. T. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med. Sci. Sports Exerc. 32 (1), 70–84 (2000).
Google Scholar
Niemeyer, M., Knaier, R. & Beneke, R. The oxygen uptake Plateau-A critical review of the frequently misunderstood phenomenon. Sports Med. 51 (9), 1815–1834 (2021).
Google Scholar
Taylor, H. L., Buskirk, E. & Henschel, A. Maximal oxygen intake as an objective measure of cardio-respiratory performance. J. Appl. Physiol. 8 (1), 73–80 (1955).
Google Scholar
Midgley, A. W., McNaughton, L. R., Polman, R. & Marchant, D. Criteria for determination of maximal oxygen uptake: A brief critique and recommendations for future research. Sports Med. 37 (12), 1019–1028 (2007).
Google Scholar
Glassford, R. G., Baycroft, G. H., Sedgwick, A. W. & Macnab, R. B. Comparison of maximal oxygen uptake values determined by predicted and actual methods. J. Appl. Physiol. 20 (3), 509–513 (1965).
Google Scholar
Astrand, P. O. & Saltin, B. Maximal oxygen uptake and heart rate in various types of muscular activity. J. Appl. Physiol. 16, 977–981 (1961).
Google Scholar
Wyndham, C. H., Strydom, N. B., Leary, W. P. & Williams, C. G. Studies of the maximum capacity of men for physical effort. I. A comparison of methods of assessing the maximum oxygen intake. Int. Z. Angew Physiol. 22 (4), 285–295 (1966).
Google Scholar
Millet, G. P., Vleck, V. E. & Bentley, D. J. Physiological differences between cycling and running: Lessons from triathletes. Sports Med. 39 (3), 179–206 (2009).
Google Scholar
Stromme, S. B., Ingjer, F. & Meen, H. D. Assessment of maximal aerobic power in specifically trained athletes. J. Appl. Physiol. Respir Environ. Exerc. Physiol. 42 (6), 833–837 (1977).
Google Scholar
Hermansen, L., Ekblom, B. & Saltin, B. Cardiac output during submaximal and maximal treadmill and bicycle exercise. J. Appl. Physiol. 29 (1), 82–86 (1970).
Google Scholar
Hermansen, L. & Saltin, B. Oxygen uptake during maximal treadmill and bicycle exercise. J. Appl. Physiol. 26 (1), 31–37 (1969).
Google Scholar
Brink-Elfegoun, T., Holmberg, H. C., Ekblom, M. N. & Ekblom, B. Neuromuscular and circulatory adaptation during combined arm and leg exercise with different maximal work loads. Eur. J. Appl. Physiol. 101 (5), 603–611 (2007).
Google Scholar
Langeskov-Christensen, M., Langeskov-Christensen, D., Overgaard, K., Møller, A. B. & Dalgas, U. Validity and reliability of VO2-max measurements in persons with multiple sclerosis. J. Neurol. Sci. 342 (1–2), 79–87 (2014).
Google Scholar
Pivarnik, J. M., Dwyer, M. C. & Lauderdale, M. A. The reliability of aerobic capacity (VO2max) testing in adolescent girls. Res. Q. Exerc. Sport. 67 (3), 345–348 (1996).
Google Scholar
Day, J. R., Rossiter, H. B., Coats, E. M., Skasick, A. & Whipp, B. J. The maximally attainable VO2 during exercise in humans: The peak vs. maximum issue. J. Appl. Physiol. (1985). 95 (5), 1901–1907 (2003).
Google Scholar
Andersen, L. B. A maximal cycle exercise protocol to predict maximal oxygen uptake. Scand. J. Med. Sci. Sports. 5 (3), 143–146 (1995).
Google Scholar
Katch, V. L., Sady, S. S. & Freedson, P. Biological variability in maximum aerobic power. Med. Sci. Sports Exerc. 14 (1), 21–25 (1982).
Google Scholar
Beltz, N. M. et al. Graded exercise testing protocols for the determination of VO(2)max: Historical perspectives, progress, and future considerations. J. Sports Med. (Hindawi Publ Corp). 2016, 3968393 (2016).
Google Scholar
Van Hooren, B., Souren, T. & Bongers, B. C. Accuracy of respiratory gas variables, substrate, and energy use from 15 CPET systems during simulated and human exercise. Scand. J. Med. Sci. Sports. 34 (1), e14490 (2024).
Google Scholar
Vaccaro, P. & Mahon, A. Cardiorespiratory responses to endurance training in children. Sports Med. 4 (5), 352–363 (1987).
Google Scholar
Astrand, I., Astrand, P. O., Hallbäck, I. & Kilbom, A. Reduction in maximal oxygen uptake with age. J. Appl. Physiol. 35 (5), 649–654 (1973).
Google Scholar
Walsh, J., Walsh, R. & Redmond, K. Systematic review of physiological and psychological outcomes of surgery for pectus excavatum supporting commissioning of service in the UK. BMJ Open. Respir Res. ;10(1). (2023).
Casar Berazaluce, A. M. et al. The chest wall gender divide: Females have better cardiopulmonary function and exercise tolerance despite worse deformity in pectus excavatum. Pediatr. Surg. Int. 36 (11), 1281–1286 (2020).
Google Scholar
Dupuis, M. et al. Impact of pectus excavatum on pulmonary function and exercise capacity in patients treated with 3D custom-made silicone implants. Ann. Chir. Plast. Esthet. 69 (1), 53–58 (2024).
Google Scholar
Jensen, K., Johansen, L. & Secher, N. H. Influence of body mass on maximal oxygen uptake: Effect of sample size. Eur. J. Appl. Physiol. 84 (3), 201–205 (2001).
Google Scholar
Haecker, F. M. & Sesia, S. B. Intraoperative use of the vacuum bell for elevating the sternum during the Nuss procedure. J. Laparoendosc. Adv. Surg. Tech. A. 22 (9), 934–936 (2012).
Google Scholar
Kar, A., Baghai, M. & Hunt, I. Reshaping the evidence for surgical correction of pectus excavatum using cardiopulmonary exercise testing. J. Am. Heart Assoc. 11 (7), e025273 (2022).
Google Scholar